What is Anthrax disease?
Last Update on September 29, 2022
| Overview | Types of Anthrax | Symptoms of Anthrax | Diagnosis | Causes of Anthrax | Risk factors | Complications | Prevention | Treatment |
1. Overview:
Anthrax disease is a deadly infectious disease that is caused by gram-positive, rod-shaped bacteria. This natural occurrence in soil has a significant impact on both domestic and wild animals all over the planet.
If people come into contact with diseased animals or tainted animal products, they could become ill with anthrax disease. Both humans and animals can get life-threatening illnesses as a result of anthrax disease.
Anthrax disease affects livestock and wild game mostly. Humans can become infected via either direct or indirect contact with sick animals.
Although grazing animals like cattle, sheep, goats, horses, and mules are the ones most frequently infected by anthrax disease, humans can contract the disease by working with an infected animal’s wool, hair, hides, bones, or carcasses. A sore with a coal-black center appears when anthrax disease, whose name is derived from the Greek word for coal, infects a person’s epidermis.
Even while there is no evidence that anthrax disease spreads from one person to another, it is feasible that the skin lesions brought on by the disease could spread through direct contact or contact with a contaminated object (fomite). Usually, a skin wound is where anthrax germs enter the body. The infection could also be carried on by eating infected meat or breathing in the spores.
Examples of signs and symptoms that change depending on how you got the infection include skin sores, vomiting, and shock. The majority of anthrax disease infections are curable with quick antibiotic treatment. Inhaling anthrax is exceedingly harmful and could be fatal.
In the developed world, anthrax disease is quite uncommon. However, the disease continues to be a hazard because the bacteria have been used in bioterrorism attacks in the US.
2. Types of Anthrax Disease:
Depending on how anthrax enters a person’s body, several illnesses might manifest. Skin, lungs, or the digestive system are the most common entry points for anthrax into the body. In the long run, if no antibiotics are used to treat them, anthrax of all kinds can spread throughout the body and result in death. There are 4 different types of Anthrax disease:
- Cutaneous anthrax
- Inhalation anthrax
- Gastrointestinal anthrax
- Injection anthrax
2.1. Cutaneous anthrax disease:
The most frequent and regarded as least hazardous type of anthrax infection is cutaneous anthrax. Typically, an infection appears one to seven days following exposure.

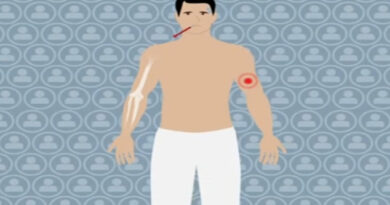
Skinned anthrax can form when anthrax spores enter the body through the skin, typically through a cut or scrape. This may occur if a person comes into contact with diseased animals or animal products like wool, skins, or hair. The head, neck, forearms, and hands are the most often affected areas by cutaneous anthrax disease. The skin and surrounding tissue are affected near the infection site.
Up to 20% of cutaneous anthrax patients pass away without receiving treatments. But with the right care, nearly all cutaneous anthrax victims survive.
2.2. Inhalation anthrax disease:
The most lethal type of anthrax disease is thought to be that which is inhaled. After exposure, infection often appears within a week, although it can take up to two months.

An individual who inhales anthrax spores may develop inhalation anthrax disease. Those who work around diseased animals or contaminated animal products from infected animals, such as in wool mills, slaughterhouses, and tanneries, may breathe in the spores. Anthrax that is inhaled initially affects the lymph nodes in the chest before spreading to other parts of the body and finally leading to severe breathing issues and shock.
anthrax disease inhalation is almost invariably lethal in the absence of therapy. However, approximately 55% of patients survive when given vigorous therapy.
2.3. Gastrointestinal anthrax disease:
Rarely have cases of gastrointestinal anthrax been documented in the US. Typically, an infection appears one to seven days following exposure.

A person may acquire gastrointestinal anthrax if they consume raw or undercooked meat from an anthrax-infected animal. Anthrax spores can impact the upper gastrointestinal tract, including the neck and esophagus, the stomach, and the intestines, resulting in a wide range of symptoms after ingestion.
More than half of patients with gastrointestinal anthrax pass away without receiving therapy. However, 60% of patients survive with the right care.
2.4. Injection anthrax disease:
Infections of this kind have never been identified in the US. In northern Europe, heroin injectors have recently been found to have another sort of anthrax infection.

Although there may be an infection deep beneath the skin or in the muscle where the medication was injected, the symptoms may be identical to those of cutaneous anthrax. Anthrax from an injection can spread more quickly throughout the body and is more difficult to diagnose and cure. A skin or injection site infection in a drug user does not always indicate that they have anthrax because many other, more prevalent bacteria can also cause these conditions.
3. Symptoms of Anthrax disease:
There are four common ways to get anthrax, and each one causes a different set of signs and symptoms. Most of the time, symptoms appear six days after being infected with the bacteria. The signs of inhalation anthrax could, however, take longer than six weeks to develop.
3.1. Symptoms of Cutaneous anthrax disease:
Anthrax disease infections that are skin-related (cutaneous) enter your body through your skin, typically through a cut or other sore. It’s by far the disease’s most prevalent pathway. And it’s the mildest. When properly treated, cutaneous anthrax disease seldom results in death. Some warning signs and symptoms are:
- An elevated, itchy bump that looks like an insect bite and swiftly transforms into a painless sore with a dark core.
- Swelling of the sore and the lymph nodes adjacent
- Flu-like symptoms, such as fever and headache, can occasionally
3.2. Symptoms of Gastrointestinal anthrax disease:
Eating undercooked meat from an infected animal can cause gastrointestinal anthrax disease infection. From your neck to your colon, it may have an impact on your digestive system. Some warning signs and symptoms are:
- Nausea
- Vomiting
- Abdominal pain
- Headache
- Loss of appetite
- Fever
- In the final stages of the illness, severe, bloody diarrhea
- Sore throat and difficulty swallowing
- Swollen neck
3.3. Symptoms of Inhalation anthrax disease:
Inhalation inhaling anthrax spores cause anthrax disease to develop. Even with therapy, it frequently results in death because it is the most lethal type of illness. Initial symptoms and indicators include:
- Sore throat
- Mild fever
- Fatigue
- Muscle aches
- Mild chest discomfort
- Shortness of breath
- Nausea
- Coughing up blood
- Painful swallowing
- High fever
- Trouble breathing
- Shock
3.4. Symptoms of Injection anthrax disease:
Only cases of anthrax disease infection from this most recent discovery have been documented outside of Europe. Through illegal drug injection, it is contracted. Initial warning indicators include:
- Redness at the area of injection
- Significant swelling
- Shock
- Multiple organ failure
- Meningitis
4. Anthrax Infection Diagnosis and Testing:
- Blood test to detect toxins or antibodies
- A sample to be examined for the presence of Bacillus anthracis
- blood
- skin lesion swab
- spinal fluid
- respiratory secretions
Chest X-rays or CT scans can determine if the patient has meditational widening or pleural effusion, which are X-ray abnormalities frequently observed in people with inhalation anthrax disease if inhalation anthrax is suspected.
5. Causes of Anthrax disease:
Anthrax spores are produced by anthrax bacteria, which are naturally found in soil on the majority of the earth. The spores might remain latent for a long time before they infect a host. Livestock, including sheep, cattle, horses, and goats, can frequently act as anthrax hosts.
Even though it is rare in the United States, anthrax disease is still common in the developing globe, especially in areas like Central America, South America, sub-Saharan Africa, Central Asia, southwest Asia, southern Europe, Eastern, the Caribbean, and Europe.
Having contact with infected animals, their meat, or their skins is the main cause of anthrax cases in people. A few Americans who used tainted animal skins to make traditional African drums have developed anthrax disease as a result.
The 2001 bioterrorism strike in the United States was one of the rare recorded instances of no animal transmission. Twenty-two people contracted anthrax after being exposed to spores that were sent through the mail, and five of them died.
More recently, heroin users in Europe who injected illegal substances became infected with anthrax disease in two different epidemics. 40 persons died in all. Most likely, the heroin that is sold in Europe originates from regions where anthrax disease occurs more frequently naturally.
6. Risk factors of Anthrax:
You must directly come into touch with anthrax spores in order to develop anthrax disease. In the event that you:
- Are serving in the military and stationed in a region where anthrax infection is highly likely
- Working in a laboratory with anthrax
- Avoid handling hair, wool, or skins from animals in anthrax-prone areas.
- If you work with cattle, consider a career in veterinary medicine.
- Handle or dress game animals – while anthrax outbreaks in domestic cattle and wild animals like deer are uncommon in the United States, they do occur occasionally.
- Injecting heroin or other illicit drugs.
7. Complications:
Anthrax’s most severe side effects include:
- Your body’s inability to adapt to infection generally causes harm to numerous organ systems.
- Meningitis, or hemorrhagic meningitis, is an infection of the membranes and fluid around the brain and spinal cord.
8. Prevention of Anthrax disease:
Most people will never be exposed to anthrax disease since it is so uncommon. Anthrax disease can be prevented by a licensed vaccination, but it is only advised for routine use in specific populations of adults who are at risk.
- A 60-day course of antibiotics is recommended, with both adults and children being able to take ciprofloxacin, doxycycline, and levofloxacin.
- Anthrax vaccination in a three-dose regimen
- Treatment with the monoclonal antibodies raxibacumab and obiltoxaximab is used in some circumstances.
8.1. Preventing anthrax during travel:
Visitors to regions where anthrax disease is prevalent or where there is an animal outbreak risk contracting the disease if they come into contact with infected animal carcasses or consume meat from sick animals.
Additionally, they run the risk of getting sick if they handle animal products or parts, including hides or drums made of animal hide. If you’re traveling through these regions, stay away from livestock, animal byproducts, and animal carcasses, and never eat raw or undercooked meat.
8.2. Preventing anthrax from animal hides:
A number of anthrax disease cases in the US have been linked to imported animal hides. Drum makers have been known to use these hides in some instances. Additionally, cases have been reported in those who touched, were close to, or were in the same area as the drums’ manufacturing.
There is no means to test for the presence of anthrax spores on imported hides, despite the fact that some may contain them.
Make sure to use hides from the following animals to avoid exposure to anthrax spores:
- United States-born animals
- Imported animals that have a global veterinary certificate proving they have undergone the necessary government inspection.
9. Treatment of Anthrax Infection:
The use of antibiotics and antitoxin are just two of the treatment options available to doctors for anthrax patients. Hospitalization is required for anthrax patients with severe cases. They can need aggressive care, such as ongoing fluid evacuation and mechanical ventilation to assist with breathing.
9.1. Antibiotics:
Antibiotics, including intravenous antibiotics, can be used to treat all forms of anthrax infection (medicine given through the vein). To have the best chance of making a full recovery, it’s essential to seek medical attention as soon as possible if someone exhibits anthrax disease symptoms. Based on the patient’s medical history, doctors will choose the medicines that are most effective at treating anthrax disease and are also best for them.
9.2. Antitoxin:
Anthrax spores may become “active” once they have entered the host. Anthrax bacteria can grow spread throughout the body, and release toxins—or poisons—when they become active. Toxins from anthrax make people very sick.
Antitoxin is one potential treatment for anthrax toxins after they have been released into the body. Antitoxins attack the body’s anthrax toxins. Antitoxin must be used in conjunction with other therapeutic alternatives by doctors.
Several different antitoxin kinds can currently be utilized to treat anthrax disease.