Type 2 Diabetes
Last Update on October 20, 2023
| What Is Type 2 Diabetes? | Symptoms | Causes | Risk Factors | Prevention | Treatments | Medicines | Complications |
1. What Is Type 2 Diabetes?
Type 2 diabetes is a long-term condition that restricts your body from properly using insulin. Insulin resistance is a phrase used to define people with type 2 diabetes.
A long-term condition known as type 2 diabetes is caused by excessively high blood glucose levels. This is the general and most common type of diabetes. Insulin is not used by the body correctly in type 2 diabetes. Your body develops insulin resistance and the pancreas produces less insulin than it once did. Your primary energy source, blood glucose, is mostly derived from the food you eat. The pancreas releases the hormone insulin, which controls the level of glucose in the blood.
A disorder in the body’s ability to control and use sugar (glucose) as fuel is type 2 diabetes. This prolonged (long-term) disease causes the bloodstream to circulate with an excessive amount of sugar. With the passing of time type 2 diabetes, cardiovascular, neurological, and immune system problems might result from higher blood sugar levels.
There are basically two interconnected issues involved in type 2 diabetes. The hormone, insulin (hormone) is not produced by your pancreas in sufficient amounts to control the flow of sugar into your cells. It causes your cells to react poorly to insulin and absorb less sugar.
Although type 1 and type 2 diabetes can develop in both childhood and adulthood, respectively. However, type 2 is more common in elderly adults. Type 2 is particularly more developed in younger people as compared to the rise in childhood obesity.
The most affected age group for type 2 diabetes is the middle age group or older. It was formerly known as adult-onset diabetes. However, due to childhood obesity, type 2 diabetes also attacks children and adolescents.
Type 2 diabetes is the most widespread type of diabetes. Around 29 million Americans people have type 2 diabetes. Another 84 million people have pre-diabetes, which is elevated blood sugar (or blood glucose) but not yet, diabetes.
Although there is no treatment for type 2 diabetes you can manage the condition by decreasing weight, eating healthfully, and exercising. You may also need medicines or insulin therapy to control your blood sugar if your diet and exercise are insufficient.
2. Symptoms of type 2 diabetes:
Type 2 diabetes symptoms and signs frequently appear slowly. In fact, you may have type 2 diabetes for years without noticing it. When occurring, signs and symptoms of type 2 diabetes are:
- Being very thirsty
- Repeating urination
- Blurry vision
- Being cranky
- Tingling
- Increased hunger
- Fatigue/feeling worn out
- Wounds that don’t heal for a longer time
- Yeast infections
- Speedily Weight loss
- Getting more infectious diseases
Consult your doctor if you have dark rashes symptoms under your arms or around your neck. These are known as acanthosis nigricans, and this type of diabetes may identify that your body is developing insulin resistance.
3. Causes of Type 2 Diabetes:
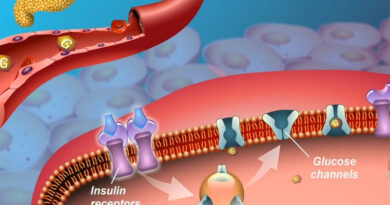
Your pancreas produces a hormone that is called insulin to control diabetes. It supports the conversion of glucose, a type of sugar from the food you eat, into energy in your cells. Insulin is produced by people with type 2 diabetes, but their cells don’t use it as effectively as they could.
Insulin resistance develops in the liver, muscle, and fat cells to use blood sugar. These cells don’t use enough blood sugar because insulin doesn’t interact with them normally.
A sufficient amount of insulin cannot be released by the pancreas to control blood sugar levels in the body.
Your pancreas initially produces more insulin in an effort to get glucose into your cells. But ultimately it can’t keep up, and your blood starts to become thick with glucose.
Usually, a number of factors work together to develop type 2 diabetes. They could consist of:
- Genes: Researchers have discovered certain DNA segments that have an impact on how your body produces insulin.
- Extra gain weight: Insulin resistance can be caused by being overweight or obese, particularly if you carry excess weight around your abdomen.
- Metabolic syndrome: High blood sugar, additional body fat around the belly, high blood pressure, high cholesterol, and high triglycerides are all common symptoms of insulin resistance.
- High glucose release liver: When you have low blood sugar, your liver produces and releases glucose. Your blood sugar rises after eating, and your liver often slows down and stores its glucose for later. However, not everyone’s livers do. They continue producing sugar.
- Weak communication between cells: Cells frequently transmit incorrect signals or fail to correctly pick up communications. Diabetes can develop as a result of a series of issues that influence the production and usage of insulin and glucose by your cells.
- Damage beta cells: Your blood sugar is put off if the cells that produce insulin release the incorrect dosage of insulin at the incorrect time. Beta cells can also become damaged by high blood sugar.
Although the exact cause of this is uncertain, being overweight and being inactive are major risk factors.
4. Risk Factors of Type 2 Diabetes:
There are some factors that increase your risk of developing type 2 diabetes. Your chances of receiving it are higher the more of these apply to you. Several things have to do with what you are:
- Age: 45 years or older
- Family: Diabetes in a parent, sister, or brother
- Ethnicity: American citizens who consider African American, Alaska Native, Native American, Asian, Hispanic or Latino, or Pacific Islander.
Your health and medical background are risk factors that include:
- Being overweight quickly: Obesity or being overweight is a major risk.
- Family medical background: If your parent or sibling has type 2 diabetes, your risk of developing it also rises.
- Physically inactivity: Your risk increases the less active you stay. Exercise benefits weight management burns glucose as fuel, and increases insulin sensitivity in your cells.
- Diffusion of fat: A higher risk is identified if you store fat primarily in your abdomen rather than your hips and thighs. A male with a waist measurement above 40 inches or a woman with a waist measurement over 35 inches, you have a higher risk of developing type 2 diabetes.
- Low HDL: Low levels of high-density lipoprotein (HDL) cholesterol, or the “good” cholesterol, and high levels of triglycerides are linked to greater risk.
- Pre-diabetes: A blood sugar level that is greater than usual but not high enough to be classified as diabetes is called pre-diabetes. Pre-diabetes frequently develops into type 2 diabetes if left untreated.
- Pregnancy issues: If you had gestational diabetes while pregnant or had a baby that weighed more than 9 pounds, your chance of getting type 2 diabetes is higher.
- Polycystic ovary syndrome: The risk of diabetes is increased with polycystic ovary syndrome. It is a common disease marked by irregular menstrual cycles, excessive hair growth, and obesity.
- Heart and blood vessel disease: Type 2 diabetes may create problems for the Heart and blood vessels.
- Depression: Major depressive disorder, commonly known as depression, is a mood disease that causes you to feel permanently down or bored in life.
5. Prevention of type 2 diabetes:
Maintaining a healthy lifestyle can help control diabetes, even if you have blood relatives who suffer from the condition. Changes in your way of life may slow or stop the development of diabetes if you have been diagnosed with pre-diabetes.
A healthy way of life comprises:
- Eating healthy foods: Eat foods with more fiber and lower calories and fat. Keep a focus on fruits, vegetables, and whole grains in your meal.
- Doing physical activities: Regular exercise for 30 minutes will reduce your risk of getting type 2 diabetes by approximately a third.
- Decrease your weight: The transition from pre-diabetes to type 2 diabetes can be halted by modest weight loss and weight maintenance. Losing 7% to 10% of your body weight can lower your chance of developing diabetes if you have pre-diabetes.
- Avoiding inactivity for long periods: Your risk of type 2 diabetes may rise if you spend a lot of time sitting still. Try to get up and move around for at least a few minutes every 30 minutes.
- Stop smoking: Smoking leads to an increase in the chance of getting type 2 diabetes.
6. Treatments for type 2 diabetes:
A combination of medication and lifestyle modifications are used to control type 2 diabetes.
6.1. Lifestyle changes:
You might be able to control your blood sugar levels only with diet and exercise.
- Weight loss: Losing extra weight can be good. While decreasing 5% of your body weight is beneficial, it seems optimal to lose at least 7% of it and keep it off. In other words, losing around 13 pounds for a 180-pound person can reduce blood sugar levels.
- Healthy eating: Diabetes type 2 does not have a special diet. A qualified nutritionist can educate you on carbohydrates and help you in creating a meal plan that you can follow. Consider regarding:
- Eating food with lower calories
- Stop the use of refined carbs, especially sweets products.
- Adding vegetables and fruits to your meal plan.
- Getting more fiber
- Exercise: Spend between 30 and 60 minutes per day exercising. Walking, riding, swimming, and other activities that raise your heart rate all count as types of exercise. You can also add strength training exercises like weightlifting or yoga can be added to that. If you take medication to reduce blood sugar, you may need to eat before working out.
- Monitoring your blood sugar levels: Your doctor may advise you to test your blood sugar levels regularly. Monitoring your blood sugar depends on your treatment, particularly if you are using insulin.
6.2. Medicines for type 2 diabetes:
You could need medication if changing your way of life doesn’t help you reach your goal blood sugar levels. The most typical symptoms of type 2 diabetes include:
- Metformin
- Sulfonylureas
- Meglitinides
- Thiazolidinediones
- DPP-4 inhibitors
- GLP-1 receptor agonists
- SGLT2 inhibitors
- GIP and GLP-1 receptor agonist
- Insulin
It’s possible that your blood sugar will continue to worsen over time, even if you make lifestyle changes and take your medication as prescribed. That doesn’t mean you did something wrong in any way. Over time, many people have a need for various drugs because diabetes gets stronger.
Combination therapy refers to the use of several drugs to treat type 2 diabetes.
Your doctor and you should work together to choose the best combination for you. You’ll typically keep taking metformin while getting anything else.
Your circumstances may determine what that is. For example, some drugs control blood sugar increase that happens soon after meals. Some people are better at preventing hypoglycemia, which is a decrease in blood sugar between meals. Some might help you manage your diabetes, weight, or cholesterol.
It is really possible that using a second medicine won’t support blood sugar control. The combined effects of the two medications might only last a short time. In that situation, your doctor may advise starting insulin therapy or prescribing a third non-insulin drug.
7. Complications:
Various vital organs, including your heart, blood arteries, nerves, eyes, and kidneys, are impacted by type 2 diabetes. Additionally, diabetes risk factors raise the possibility of developing other serious chronic diseases. By managing your diabetes and controlling your blood sugar, you can lower your chance of these effects or associated diseases.
Diabetes and other common co-morbidities could result in the following complications:
- Blood vessel and heart disease: Diabetes is linked to a higher chance of heart disease, stroke, hypertension, and blood vessel narrowing (atherosclerosis).
- Limb nerve injury: Over time, high blood sugar can harm or kill nerves, causing tingling, numbness, burning, pain, or even ultimate loss of feeling. The typical development of these symptoms across the body begins at the tips of the fingers or toes.
- Further nerve damage: The heart’s nerves may have been damaged, which could be the cause of abnormal cardiac rhythms. Damage to the nerves of the digestive system may cause problems with nausea, vomiting, diarrhea, or constipation. Nerve damage may cause erectile dysfunction in men.
- Kidney failure: Dialysis or a kidney transplant may be necessary if diabetes results in chronic renal disease or irreversible end-stage kidney disease.
- Apneic sleep: Obstructive sleep apnea is typically present in people with type 2 diabetes. The primary cause of these conditions may be obesity. The relationship between treating sleep apnea and improved blood sugar control is unclear.
- Dementia: People with type 2 diabetes appear to be more vulnerable to dementia disorders including Alzheimer’s and other types of dementia. Uncontrolled blood sugar levels are linked to memory loss and other cognitive disorders more quickly. e prone to bacterial and fungal infections, among others.
- Eye problems: Diabetes may harm the blood vessels in the retina, potentially resulting in blindness, and also raises the risk of significant eye conditions such as cataracts and glaucoma.
- Skin problems: Among other skin problems, diabetes may increase your risk of bacterial and fungal infections.
- Slow healing: Slow recovery cuts and blisters can develop into dangerous infections that may not heal properly if left untreated. In cases of serious injuries, amputations of the toe, foot, or leg may be needed.
- Impairment of hearing: Hearing problems are more common in people with diabetes.